Chapter 12. INFLAMMATORY DISEASES OF THE FEMALE GENITAL ORGANS
Chapter 12. INFLAMMATORY DISEASES OF THE FEMALE GENITAL ORGANS
Inflammatory diseases of the genital organs (IGDO) in women occupy 1st place in the structure of gynecological pathology and account for 60-65% of visits to antenatal clinics. Perhaps the number of sick people is higher, since often with erased forms, patients do not go to the doctor. The increase in the number of VZPOs in all countries of the world is a consequence of changes in the sexual behavior of young people, environmental damage and decreased immunity.
Classification. Based on the localization of the pathological process, inflammatory diseases of the lower (vulvitis, bartholinitis, colpitis, endocervicitis, cervicitis) and upper (endomyometritis, salpingoophoritis, pelvioperitonitis, parametritis) parts of the genital organs, the border of which is the internal uterine pharynx, are distinguished.
According to the clinical course, inflammatory processes are divided into:
Acute with severe clinical symptoms;
Subacute with erased manifestations;
Chronic (with an unknown duration of the disease or a duration of more than 2 months) in the stage of remission or exacerbation.
Etiology. VPOs can occur under the influence of mechanical, thermal, chemical factors, but the most significant is infectious. Depending on the type of pathogen, VZPOs are divided into nonspecific and specific (gonorrhea, tuberculosis, diphtheria). The cause of nonspecific inflammatory diseases can be streptococci, staphylococci, enterococci, Candida fungi, chlamydia, mycoplasma, ureaplasma, Escherichia coli, Klebsiella, Proteus, viruses, actinomycetes, trichomonas, etc. Along with absolute pathogens (gonococci, chlamydia, trichomonas, Mycoplasma genitalium) Opportunistic microorganisms that live in certain areas of the genital tract, as well as associations of microorganisms, also play an important role in the occurrence of VZPO. Currently, inflammatory diseases in the genital tract are caused by mixed microflora with a predominance of anaerobic non-spore-forming microorganisms. Pathogenic pathogens of VZPO are transmitted sexually, less often - through household contact (mainly in girls when using common hygiene items). Sexually transmitted diseases include gonorrhea, chlamydia, trichomoniasis, herpes and human papillomavirus infections, acquired immunodeficiency syndrome (AIDS), syphilis, anogenital warts, and molluscum contagiosum. Opportunistic
microorganisms become pathogens of VZPO under certain conditions that increase their virulence, on the one hand, and reduce the immunobiological properties of the macroorganism, on the other.
Factors that prevent the entry and spread of infection in the body. In the genital tract there are many levels of biological protection against the occurrence of infectious diseases. The first refers to the closed state of the genital slit.
The activation of opportunistic microorganisms and the spread of infection are prevented by the properties of the vaginal microflora - the creation of an acidic environment, the production of peroxides and other antimicrobial substances, inhibition of adhesion for other microorganisms, activation of phagocytosis and stimulation of immune reactions.
Normally, the vaginal microflora is very diverse. It is represented by gram-positive and gram-negative aerobes, facultative and obligate anaerobic microorganisms. A large role in the microbiocenosis belongs to lacto- and bifidobacteria (Dederlein's bacilli), which create a natural barrier to pathogenic infection (Fig. 12.1). They make up 90-95% of the vaginal microflora in the reproductive period. By breaking down glycogen contained in the surface cells of the vaginal epithelium into lactic acid, lactobacilli create an acidic environment (pH 3.8-4.5), which is destructive for many microorganisms. The number of lactobacilli and, accordingly, the formation of lactic acid decrease with a decrease in the level of estrogen in the body (in girls in the neutral period, postmenopause). The death of lactobacilli occurs as a result of the use of antibiotics, douching of the vagina with solutions of antiseptic and antibacterial drugs. The vaginal rod-shaped bacteria also include actinomycetes, corynebacteria, bacteroids, fusobacteria.
The second place in the frequency of detection of bacteria in the vagina belongs to cocci - epidermal staphylococcus, hemolytic and non-hemolytic streptococci, enterococci. In small quantities and less often
Rice. 12.1. Microscopy of a vaginal smear. Vaginal epithelial cell against the background of lactobacteria
Enterobacteriaceae, Escherichia coli, Klebsiella, mycoplasma and ureaplasma are found, as well as yeast-like fungi of the genus Candida. Anaerobic flora predominates over aerobic and facultative anaerobic flora. The vaginal flora is a dynamic, self-regulating ecosystem.
Common infectious diseases accompanied by decreased immunity, endocrine disorders, the use of hormonal and intrauterine contraceptives, and the use of cytostatics disrupt the qualitative and quantitative composition of the vaginal microflora, which facilitates the invasion of pathogenic microorganisms and can lead to the development of inflammatory processes caused by opportunistic bacteria.
The cervical canal serves as a barrier between the lower and upper genital tracts, and the border is the internal os of the uterus. Cervical mucus contains biologically active substances in high concentrations. Cervical mucus ensures the activation of nonspecific protective factors (phagocytosis, synthesis of opsonins, lysozyme, transferrin, harmful to many bacteria) and immune mechanisms (complement system, immunoglobulins, T-lymphocytes, interferons). Hormonal contraceptives cause thickening of the cervical mucus, which becomes difficult for infectious agents to pass through.
The spread of infection is also prevented by the rejection of the functional layer of the endometrium during menstruation, along with the microorganisms that have entered there. When an infection penetrates into the abdominal cavity, the plastic properties of the pelvic peritoneum help to limit the inflammatory process to the pelvic area.
Ways of spread of infection. The spread of infection from the lower genital tract to the upper genital tract can be passive or active. Passive includes spread through the cervical canal into the uterine cavity, into the tubes and abdominal cavity, as well as the hematogenous or lymphogenic route. Microorganisms can also be actively transported on the surface of moving sperm and trichomonas.
The spread of infection in the genital tract is facilitated by:
Various intrauterine manipulations, during which infection is introduced from the external environment or from the vagina into the uterine cavity, and then the infection enters through the fallopian tubes into the abdominal cavity;
Menstruation, during which microorganisms easily penetrate from the vagina into the uterus, causing an ascending inflammatory process;
Childbirth;
Surgeries on the abdominal and pelvic organs;
Foci of chronic infection, metabolic and endocrine disorders, insufficiency or imbalance of nutrition, hypothermia, stress, etc.
Pathogenesis. After infection penetrates, destructive changes occur in the lesion with the occurrence of an inflammatory reaction. Biologically active inflammatory mediators are released, causing microcirculation disorders with exudation and at the same time stimulating proliferative processes. Along with local manifestations of the inflammatory reaction, characterized by five cardinal effects,
signs (redness, swelling, fever, pain and dysfunction) may cause general reactions, the severity of which depends on the intensity and extent of the process. General manifestations of inflammation include fever, reactions of hematopoietic tissue with the development of leukocytosis, increased ESR, accelerated metabolism, and intoxication of the body. The activity of the nervous, hormonal and cardiovascular systems, the indicators of immunological reactivity of the hemostasiogram change, and microcirculation is disrupted at the site of inflammation. Inflammation is one of the most common pathological processes. With the help of inflammation, localization and then elimination of the infectious agent along with the tissue damaged under its influence is ensured.
12.1. Inflammatory diseases of the lower genital tract
Vulvitis- inflammation of the external genitalia (vulva). In women of the reproductive period, vulvitis often develops secondarily - with colpitis, endocervicitis, endometritis, adnexitis. Primary vulvitis occurs in adults with diabetes, poor hygiene (diaper rash due to obesity), thermal, mechanical (injuries, abrasions, scratching), and chemical effects on the skin of the external genitalia.
In acute vulvitis, patients complain of itching, burning in the external genital area, and sometimes of general malaise. Clinically, the disease is manifested by hyperemia and swelling of the vulva, purulent or serous-purulent discharge, and enlarged inguinal lymph nodes. In the chronic stage, clinical manifestations subside, itching and burning appear periodically.
Additional methods for diagnosing vulvitis include bacterioscopic and bacteriological examination of the discharge of the external genital organs to identify the causative agent of the disease.
Treatment vulvitis consists in eliminating the concomitant pathology that caused it. Vaginal lavage is prescribed with an infusion of herbs (chamomile, calendula, sage, St. John's wort), antiseptic solutions (dioxidine ♠, miramistin ♠, chlorhexidine, octenisept ♠, potassium permanganate, etc.). They use complex antibacterial drugs that are effective against many pathogenic bacteria, fungi, trichomonas: polyzhi-nax ♠, terzhinan ♠, neo-penotran ♠, nifuratel (macmiror ♠) for insertion into the vagina daily for 10-14 days. Ointments with antiseptics or antibiotics are applied to the vulva area. After inflammatory changes have subsided, ointments with retinol, vitamin E, solcoseryl ♠, Acto-vegin ♠, sea buckthorn oil, rosehip oil, etc. can be used topically to accelerate reparative processes. Physiotherapy is also used: ultraviolet irradiation of the vulva, laser therapy. For severe itching of the vulva, antihistamines (diphenhydramine, chloropyramine, clemastine, etc.) and local anesthetics (anesthetic ointment) are prescribed.
Bartholinitis- inflammation of the large gland of the vestibule of the vagina. The inflammatory process in the columnar epithelium lining the gland and surrounding tissues quickly leads to blockage of its excretory duct with the development of an abscess.
With bartholinitis, the patient complains of pain at the site of inflammation. Hyperemia and swelling of the excretory duct of the gland are determined, and when pressed, purulent discharge appears. The formation of an abscess leads to a worsening of the condition. Weakness, malaise, headache, chills, an increase in body temperature up to 39 ° C appear, pain in the Bartholin gland area becomes sharp and throbbing. Upon examination, swelling and hyperemia are visible in the middle and lower thirds of the labia majora and minora on the affected side, as well as a tumor-like formation covering the entrance to the vagina. Palpation of the formation is sharply painful. Surgical or spontaneous opening of the abscess helps to improve the condition and gradual disappearance of the symptoms of inflammation. The disease can recur, especially with self-medication.
Treatment Bartholinitis comes down to the use of antibiotics, taking into account the sensitivity of the pathogen, and symptomatic remedies. Local applications of anti-inflammatory ointments (levomekol ♠) and application of an ice pack are prescribed to reduce the severity of inflammation. In the acute phase of the inflammatory process, physiotherapy is used - UHF on the area of the affected gland.
When an abscess forms in the Bartholin gland, surgical treatment is indicated - opening the abscess with the formation of an artificial duct by suturing the edges of the mucous membrane of the gland to the edges of the skin incision (marsupialization). After the operation, the sutures are treated with antiseptic solutions for several days.
12.2. Infectious diseases of the vagina
Infectious diseases of the vagina are the most common in patients during the reproductive period. These include:
Bacterial vaginosis;
Nonspecific vaginitis;
Vaginal candidiasis;
Trichomonas vaginitis.
According to modern concepts, the development of an infectious disease of the vagina occurs as follows. After adhesion to the epithelial cells of the vagina, opportunistic microorganisms begin to actively multiply, which causes the occurrence of vaginal dysbiosis. Subsequently, as a result of overcoming the protective mechanisms of the vagina, infectious agents cause an inflammatory reaction (vaginitis).
Bacterial vaginosis (BV) is a non-inflammatory clinical syndrome caused by the replacement of lactobacilli in the vaginal flora by opportunistic anaerobic microorganisms. Currently, BV is considered not as a sexually transmitted infection, but as a vaginal
nal dysbiosis. At the same time, BV creates the prerequisites for the occurrence of infectious processes in the vagina, so it is considered together with inflammatory diseases of the genital organs. BV is a fairly common infectious disease of the vagina, found in 21-33% of patients of reproductive age.
Etiology and pathogenesis. Previously, the cause of the disease was considered to be gardnerella, which is why it was called gardnerellosis. However, it was later found that Gardnerella vaginalis- not the only causative agent of BV; in addition, this microorganism is an integral part of the normal microflora. Violation of the microecology of the vagina is expressed in a decrease in the number of lactobacilli that dominate normally and the rapid proliferation of various bacteria (Gardnerella vaginalis, Mycoplasma hominis), but above all - obligate anaerobes (Bacteroides spp., Prevotella spp., Peptostreptococcus spp., Mobiluncus spp., Fusobacterium spp. and etc.). Not only the qualitative, but also the quantitative composition of the vaginal microflora changes with an increase in the total concentration of bacteria.
The disease is predisposed by the use of antibacterial drugs, including antibiotics, the use of oral contraceptives and the use of IUDs, hormonal disorders with the clinical picture of oligo- and opsomenorea, previous inflammatory diseases of the genital organs, frequent changes of sexual partners, decreased immunity, etc.
As a result of disruption of the vaginal microbiocenosis, the pH of the vaginal contents changes from 4.5 to 7.0-7.5, anaerobes form volatile amines with an unpleasant smell of rotten fish. The described changes disrupt the functioning of natural biological barriers in the vagina and contribute to the occurrence of inflammatory diseases of the genital organs and postoperative infectious complications.
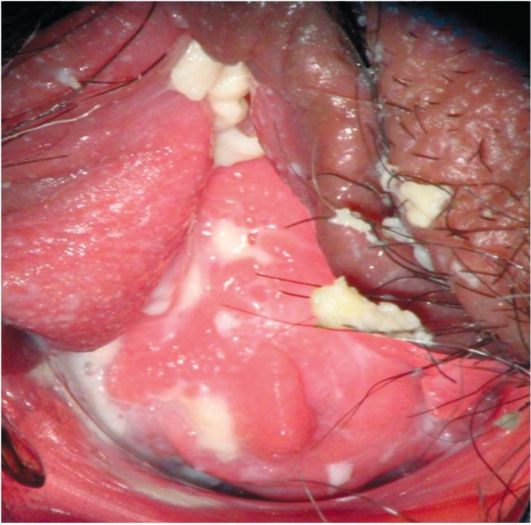
Clinical symptoms. The main complaint in patients with BV is copious, homogeneous, creamy, gray vaginal discharge that sticks to the vaginal walls (Fig. 12.2) and has an unpleasant “fishy” odor. Itching, burning in the vaginal area, and discomfort during sexual intercourse are possible.
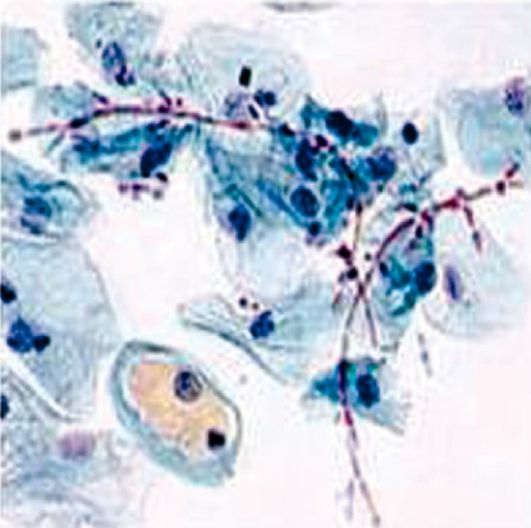
Microscopy of vaginal smears stained with Gram stain reveals “key” cells in the form of desquamated vaginal epithelial cells,

Rice. 12.2. Bacterial vaginosis
to the surface of which microorganisms characteristic of BV are attached (Fig. 12.3). In healthy women, "key" cells are not detected. In addition, typical bacterioscopic signs of the disease are a small number of leukocytes in the field of view, a decrease in the number or absence of Dederlein rods.
The diagnostic criteria for BV (Amsel criteria) are:
Specific vaginal discharge;
Detection of “key” cells in a vaginal smear;
pH of vaginal contents >4.5;
Positive amine test (smell of rotten fish when potassium hydroxide is added to vaginal secretions).
The diagnosis of BV can be made if three of the listed criteria are present. Diagnostics is complemented by a bacteriological research method with determination of the qualitative and quantitative composition of the vaginal microflora, as well as a microscopic assessment of the relative proportion of bacterial morphotypes in the vaginal smear (Nugent criterion).
Treatment male sexual partners for the purpose of preventing relapses of bacterial vaginosis in women is not advisable. However, in men, urethritis cannot be ruled out, which requires examination and, if necessary, treatment. The use of condoms during treatment is not necessary.
Therapy consists of metronidazole, ornidazole, or clindamycin orally or intravaginally for 5-7 days. It is possible to use Terzhinan ♠, nifuratel in the form of vaginal tablets or suppositories for 8-10 days.
After antibacterial therapy, measures are indicated to restore normal vaginal microbiocenosis with the help of eubiotics - Vagilak ♠, Lactobacterin ♠, Bifidumbacterin ♠, Acylact ♠, etc. The use of vitamins and biogenic stimulants aimed at increasing the overall resistance of the body is also recommended.
For immunotherapy and immunoprophylaxis of BV, the SolkoTrichovak ♠ vaccine was created, consisting of special strains of lactobacilli. Antibodies formed as a result of vaccine administration effectively uni-

Rice. 12.3. Microscopy of a vaginal smear. "Key" cell
They eliminate pathogens of the disease, normalizing the vaginal microflora, and create immunity that prevents relapses.
Nonspecific vaginitis (colpitis)- inflammation of the vaginal mucosa, caused by various microorganisms, can occur as a result of chemical, thermal, mechanical factors. Among the causative agents of vaginitis, the most important is opportunistic flora, primarily staphylococci, streptococci, Escherichia coli, and non-spore-forming anaerobes. The disease occurs as a result of an increase in the virulence of saprophytic microorganisms of the vagina with a decrease in the immunobiological defense of the macroorganism.
In the acute stage of the disease, patients complain of itching, burning in the vagina, purulent or serous-purulent discharge from the genital tract, pain in the vagina during sexual intercourse (dyspareunia). Vaginitis is often combined with vulvitis, endocervicitis, and urethritis. During a gynecological examination, attention is drawn to swelling and hyperemia of the vaginal mucosa, which bleeds easily when touched, purulent deposits and pinpoint hemorrhages on its surface. In severe cases of the disease, desquamation of the vaginal epithelium occurs with the formation of erosions and ulcers. In the chronic stage, itching and burning become less intense and occur periodically; the main complaint remains about serous-purulent discharge from the genital tract. Hyperemia and swelling of the mucous membrane decrease; in places of erosion, infiltrates of the papillary layer of the vagina can form, detected in the form of point elevations above the surface (granular colpitis).
An additional method for diagnosing vaginitis is colposcopy, which helps to detect even mild signs of the inflammatory process. To identify the causative agent of the disease, bacteriological and bacterioscopic examination of discharge from the vagina, urethra, and cervical canal is used. Microscopy of a vaginal smear reveals a large number of leukocytes, desquamated epithelial cells, and abundant gram-positive and gram-negative flora.
Treatment treatment of vaginitis should be comprehensive, aimed, on the one hand, at fighting the infection, and on the other, at eliminating concomitant diseases and increasing the body's defenses. Etiotropic therapy consists of prescribing antibacterial drugs that affect the causative agents of the disease. For this purpose, both local and general therapy are used. Vaginal rinsing or douching is prescribed with solutions of dioxidine ♠, chlorhexidine, betadine ♠, miramistin ♠, chlorophyllipt ♠ 1-2 times a day. Long-term douching (more than 3-4 days) is not recommended, as it interferes with the restoration of the natural biocenosis and normal acidity of the vagina. For senile colpitis, it is advisable to use estrogens topically, which help increase the biological protection of the epithelium (estriol - ovestine ♠ in suppositories, ointments).
Antibiotics and antibacterial agents are used in the form of suppositories, vaginal tablets, ointments, and gels. Complex drugs with antimicrobial, antiprotozoal and antifungal action - terzhinan ♠, polyzhi-nax ♠, neo-penotran ♠, nifuratel, ginalgin ♠ - have become widespread for the treatment of vaginitis. For anaerobic and mixed infections, betadine ♠, metronidazole, clindamycin, ornidazole are effective. Local treatment is often combined with general antibiotic therapy, taking into account the sensitivity of the pathogen.
After antibacterial therapy, it is necessary to prescribe eubiotics (vagilac ♠, bifidumbacterin ♠, lactobacterin ♠, biovestin ♠), which restore the natural microflora and acidity of the vagina.
Vaginal candidiasis is one of the most common diseases of the vagina of infectious etiology, its frequency has increased in recent years. In the United States, 13 million episodes of the disease are recorded every year - in 10% of the country's female population; 3 out of 4 women of reproductive age have experienced vaginal candidiasis at least once.
Etiology and pathogenesis. The causative agent of the disease is yeast-like fungi of the genus Candida. Most often (85-90%) the vagina is affected by fungi Candida albicans less often - Candida glabrata, Candida tropicalis, Candida krusei etc. Fungi of the genus Candida are single-celled aerobic microorganisms. They form pseudomycelium in the form of chains of elongated cells, as well as blastospores - budding cells in places where the pseudomycelium branches, which are elements of reproduction. Optimal conditions for the growth and reproduction of mushrooms are a temperature of 21-37 °C and a slightly acidic environment.
Genital candidiasis is not a sexually transmitted disease, but is often a marker of it. Fungi belong to the opportunistic flora that normally lives on the surface of the skin and mucous membranes, including the vagina. However, under certain conditions (decrease in general and local resistance, taking antibiotics, oral contraceptives, cytostatics and glucocorticosteroids, diabetes mellitus, tuberculosis, malignant neoplasms, chronic infections, etc.) it can cause disease. This increases the adhesive properties of fungi, which attach to vaginal epithelial cells, causing colonization of the mucous membrane and the development of an inflammatory reaction. Typically, candidiasis affects only the superficial layers of the vaginal epithelium. In rare cases, the epithelial barrier is overcome and the pathogen invades the underlying tissues with hematogenous dissemination.
According to the data obtained, when urogenital candidiasis recurs, the main reservoir of infection is the intestine, from where the fungi periodically enter the vagina, causing an exacerbation of the inflammatory process.
There are acute (duration of the disease up to 2 months) and chronic (recurrent; duration of the disease - more than 2 months) urogenital candidiasis.
Clinic. Vaginal candidiasis causes complaints of itching, burning in the vagina, and cheesy discharge from the genital tract. Itching and burning intensify after water procedures, sexual intercourse or during sleep. Involvement of the urinary tract in the process leads to dysuric disorders.
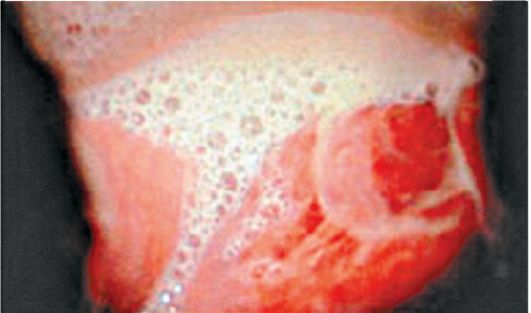
In the acute period of the disease, the skin of the external genitalia is secondarily involved in the inflammatory process. Vesicles form on the skin, which open and leave erosions. Examination of the vagina and vaginal portion of the cervix using speculum reveals hyperemia, edema, white or gray-white cheesy deposits on the vaginal walls (Fig. 12.4). Colposcopic signs of vaginal candidiasis after staining with Lugol's solution* include small pinpoint inclusions in the form of “semolina” with a pronounced vascular pattern. In the chronic course of candidiasis, secondary elements of inflammation predominate - tissue infiltration, sclerotic and atrophic changes.
The most informative diagnostic test is microbiological testing. Microscopy of a native or Gram-stained vaginal smear allows detection of spores and pseudomycelium of the fungus. A good addition to microscopy is the cultural method - sowing vaginal contents on artificial nutrient media. A cultural study makes it possible to establish the species of fungi, as well as their sensitivity to antimycotic drugs (Fig. 12.5).
Additional methods for vaginal candidiasis include examination of intestinal microbiocenosis, examination for sexually transmitted infections, and analysis of the glycemic profile with load.
Rice. 12.4. Discharge from the genital tract due to candidiasis
Rice. 12.5. Microscopy of a vaginal smear
Treatment vaginal candidiasis should be comprehensive, not only with an impact on the causative agent of the disease, but also with the elimination of predisposing factors. It is recommended to avoid taking oral contraceptives, antibiotics, and, if possible, glucocorticosteroids, cytostatics, and carry out drug correction of diabetes mellitus. During the period of treatment and clinical observation, the use of condoms is recommended.
To treat acute forms of urogenital candidiasis, at the first stage, one of the drugs is usually used locally in the form of cream, suppositories, vaginal tablets or balls: econazole, isoconazole, clotrimazole, butoconazole (Gynofort ♠), natamycin (pimafucin ♠), ketoconazole, terzhinan ♠ , nifuratel, etc. for 6-9 days. For chronic urogenital candidiasis, along with local treatment, systemic drugs are used - fluconazole, itraconazole, ketoconazole.
Low-toxic drugs are used in children - fluconazole, nifuratel, terzhinan ♠. Special attachments on the tubes allow you to apply the cream without damaging the hymen.
At the second stage of treatment, the disturbed vaginal microbiocenosis is corrected.
The criterion for cure is the resolution of clinical manifestations and negative results of microbiological examination. If treatment is ineffective, it is necessary to repeat the course using other regimens.
Prevention vaginal candidiasis is to eliminate the conditions for its occurrence.
Trichomonas vaginitis is one of the most common sexually transmitted infectious diseases and affects 60-70% of sexually active women.
Etiology and pathogenesis. The causative agent of trichomoniasis is Trichomonas vaginalis (Trichomonas vaginalis)- the simplest oval-shaped microorganism; has from 3 to 5 flagella and an undulating membrane, with the help of which it moves (Fig. 12.6). Nutrition is carried out by endosmosis and phagocytosis. Trichomonas is unstable in the external environment and easily dies when heated above 40 °C, dried, or exposed to disinfectant solutions. Trichomonas are often companions to other sexually transmitted infections (gonorrhea, chlamydia, viral infections, etc.) and (or) causing inflammation of the genital organs (yeast, mycoplasma, ureaplasma). Trichomoniasis is considered a mixed protozoan-bacterial infection.

Rice. 12.6. Microscopy of a vaginal smear. Trichomonas
Trichomonas can reduce sperm motility, which is one of the causes of infertility.
The main route of infection with trichomoniasis is sexual. The contagiousness of the pathogen is approaching 100%. The domestic route of infection is also not excluded, especially in girls, when using shared linen, bed, as well as intranatally during the passage of the fetus through the infected birth canal of the mother.
Trichomonas are found mainly in the vagina, but can affect the cervical canal, urethra, bladder, and excretory ducts of the large glands of the vestibule of the vagina. Trichomonas can penetrate through the uterus and fallopian tubes even into the abdominal cavity, carrying pathogenic microflora on its surface.
Despite the specific immunological reactions to the introduction of Trichomonas, immunity does not develop after suffering from trichomoniasis.
Classification. There are fresh trichomoniasis (disease duration up to 2 months), chronic (sluggish forms with a disease duration of more than 2 months or with an unknown duration) and trichomonas carriage, when the pathogens do not cause an inflammatory process in the genital tract, but can be transmitted to a partner through sexual contact. Fresh trichomoniasis can be acute, subacute or torpid (asymptomatic). Urogenital trichomoniasis is also divided into uncomplicated and complicated.
Clinical symptoms. The incubation period for trichomoniasis ranges from 3-5 to 30 days. The clinical picture is determined, on the one hand, by the virulence of the pathogen, and on the other, by the reactivity of the macroorganism.
In acute and subacute trichomoniasis, patients complain of itching and burning in the vagina, abundant foamy gray-yellow discharge from the genital tract (Fig. 12.7). Foamy discharge is associated with the presence of gas-forming bacteria in the vagina. Damage to the urethra causes pain when urinating
Rice. 12.7. Foamy vaginal discharge due to trichomoniasis
scanning, frequent urge to urinate. In torpid and chronic diseases, complaints are not expressed or absent.
Diagnosis is helped by a carefully collected anamnesis (contacts with patients with trichomoniasis) and objective examination data. A gynecological examination reveals hyperemia, swelling of the vaginal mucosa and the vaginal portion of the cervix, foamy pus-like leucorrhoea on the vaginal walls. Colposcopy reveals petechial hemorrhages and cervical erosions. In the subacute form of the disease, signs of inflammation are weakly expressed, while in the chronic form they are practically absent.
Microscopy of vaginal smears reveals the pathogen. It is better to use a native rather than a colored preparation, since the ability to detect the movement of Trichomonas under a microscope increases the likelihood of their detection. In some cases, fluorescence microscopy is used. In recent years, the PCR method has been increasingly used to diagnose trichomoniasis. 1 week before taking the material, patients should not use anticystic drugs and stop local procedures. Successful diagnosis involves a combination of various techniques and repeated tests.
Treatment should be carried out on both sexual partners (spouses), even if trichomonas is detected in only one of them. During the period of therapy and subsequent control, sexual activity is prohibited or the use of condoms is recommended. Trichomonas carriers should also be involved in treatment.
In acute and subacute trichomoniasis, therapy comes down to prescribing one of the specific anti-trichomoniasis drugs - ornidazole, tinidazole, metronidazole. If there is no effect of treatment, changing the drug or doubling the dose is recommended.
For trichomonas vulvovaginitis in children, the drug of choice is ornidazole.
For chronic forms of trichomoniasis that are difficult to respond to conventional therapy, the SolkoTrichovak * vaccine, which includes special strains of lactobacilli isolated from the vagina of women infected with trichomoniasis, is effective. As a result of the introduction of the vaccine, antibodies are formed that destroy Trichomonas and other inflammatory pathogens that have common antigens with lactobacilli. This normalizes the vaginal microflora and creates long-term immunity that prevents relapses.
The criteria for cure of trichomoniasis are the disappearance of clinical manifestations and the absence of trichomonas in the genital tract and urine.
Prevention Trichomoniasis comes down to timely identification and treatment of patients and Trichomonas carriers, maintaining personal hygiene, and excluding casual sexual intercourse.
Endocervicitis- inflammation of the mucous membrane of the cervical canal, occurs as a result of trauma to the cervix during childbirth, abortion, diagnostic curettage and other intrauterine interventions. The affinity for the columnar epithelium of the cervical canal is especially
characteristic of gonococci, chlamydia. Endocervicitis often accompanies other gynecological diseases of both inflammatory (colpitis, endometritis, adnexitis) and non-inflammatory (ectopia, ectropion of the cervix) etiology. In the acute stage of the inflammatory process, patients complain of mucopurulent or purulent discharge from the genital tract, and, less often, of dull nagging pain in the lower abdomen. Examination of the cervix using mirrors and colposcopy reveals hyperemia and swelling of the mucous membrane around the external os, sometimes with the formation of erosions, serous-purulent or purulent discharge from the cervical canal. Chronicity of the disease leads to the development cervicitis with the involvement of the muscle layer in the inflammatory process. Chronic cervicitis is accompanied by hypertrophy and hardening of the cervix, the appearance of small cysts in the thickness of the cervix (Nabothian cysts - ovulae Nabothii).
The diagnosis of endocervicitis is helped by bacteriological and bacterioscopic examination of discharge from the cervical canal, as well as cytological examination of smears from the cervix, which makes it possible to detect cells of columnar and stratified squamous epithelium without signs of atypia, and an inflammatory leukocyte reaction.
Treatment endocervicitis in the acute phase is to prescribe antibiotics taking into account the sensitivity of the pathogens. Local treatment is contraindicated due to the risk of ascending infection.
12.3. Inflammatory diseases of the upper genital tract (pelvic organs)
endometritis- inflammation of the uterine mucosa with damage to both the functional and basal layers. Acute endometritis, As a rule, it occurs after various intrauterine manipulations - abortion, curettage, insertion of intrauterine contraceptives (IUC), as well as after childbirth. The inflammatory process can quickly spread to the muscle layer (endomyometritis), and in severe cases, affect the entire wall of the uterus (panmetritis). The disease begins acutely - with an increase in body temperature, the appearance of pain in the lower abdomen, chills, purulent or purulent discharge from the genital tract. The acute stage of the disease lasts 8-10 days and usually ends with recovery. Less commonly, the process generalizes with the development of complications (parametritis, peritonitis, pelvic abscesses, thrombophlebitis of the pelvic veins, sepsis) or inflammation becomes subacute and chronic.
A gynecological examination reveals purulent discharge from the cervical canal, an enlarged uterus of soft consistency, painful or sensitive, especially in the area of the ribs (along the large lymphatic vessels). A clinical blood test reveals leukocytosis, a shift in the leukocyte formula to the left, lymphopenia, and an increase in ESR. Ultrasound scanning reveals an enlarged uterus, a blurred boundary between the endometrium and myometrium, a change in the echogenicity of the myometrium (alternating areas of increased and decreased echo density), an expansion of the uterine cavity with hypoechoic contents and finely dispersed contents.
nary suspension (pus), and with an appropriate history - the presence of an IUD or the remains of a fertilized egg. The endoscopic picture during hysteroscopy depends on the reasons that caused endometritis. In the uterine cavity, against the background of a hyperemic, edematous mucous membrane, fragments of necrotic mucous membrane, elements of the fertilized egg, remnants of placental tissue, foreign bodies (ligatures, IUDs, etc.) can be detected.
If the outflow of the uterus is disrupted and the discharge becomes infected due to narrowing of the cervical canal by a malignant tumor, polyp, or myomatous node, pyometra - secondary purulent lesion of the uterus. There are sharp pains in the lower abdomen, purulent-resorptive fever, and chills. During a gynecological examination, there is no discharge from the cervical canal, an enlarged, round-shaped, painful body of the uterus is detected, and with ultrasound - an expansion of the uterine cavity with the presence of fluid with a suspension in it (the echostructure corresponds to pus).
Chronic endometritis occurs more often as a result of inadequate treatment of acute endometritis, which is facilitated by repeated curettage of the uterine mucosa due to bleeding, remnants of suture material after cesarean section, IUD. Chronic endometritis is a clinical and anatomical concept; the role of infection in maintaining chronic inflammation is very doubtful, however, there are morphological signs of chronic endometritis: lymphoid infiltrates, stromal fibrosis, sclerotic changes in spiral arteries, the presence of plasma cells, gland atrophy or, conversely, hyperplasia of the mucous membrane with the formation of cysts and synechiae (adhesions) . In the endometrium, the number of receptors for sex steroid hormones decreases, resulting in inferior transformation of the uterine mucosa during the menstrual cycle. The clinical course is latent. The main symptoms of chronic endometritis include menstrual irregularities - menopause or menometrorrhagia due to impaired regeneration of the mucous membrane and decreased contractility of the uterus. Patients are bothered by nagging, aching pain in the lower abdomen, serous-purulent discharge from the genital tract. Often in the anamnesis there are indications of disorders of the generative function - infertility or spontaneous abortions. Chronic endometritis can be suspected based on anamnesis, clinical picture, gynecological examination (slight enlargement and hardening of the uterine body, serous-purulent discharge from the genital tract). There are ultrasound signs of chronic inflammation of the uterine mucosa: intrauterine synechiae, defined as hyperechoic septa between the walls of the uterus, often with the formation of cavities. In addition, due to the involvement of the basal layer of the endometrium in the pathological process, the thickness of the M-echo does not correspond to the phase of the menstrual cycle. However, for final verification of the diagnosis, a histological examination of the endometrium obtained during diagnostic curettage or pipette biopsy of the uterine mucosa is required.
Salpingoophoritis (adnexitis) - inflammation of the uterine appendages (tube, ovary, ligaments), occurs in an ascending or descending manner secondary to inflammatory changes in the abdominal organs (for example, with
appendicitis) or hematogenously. With an ascending infection, microorganisms penetrate from the uterus into the lumen of the fallopian tube, involving all layers in the inflammatory process (salpingitis), and then in half of the patients - the ovary (oophoritis) along with the ligamentous apparatus (adnexitis, salpinoophoritis). The leading role in the occurrence of adnexitis belongs to chlamydial and gonococcal infections. Inflammatory exudate, accumulating in the lumen of the fallopian tube, can lead to an adhesive process and closure of the fimbrial region. Saccular formations of the fallopian tubes (sactosalpinxes) occur. The accumulation of pus in the tube leads to the formation of pyosalpinx (Fig. 12.8), serous exudate - to the formation of hydrosalpinx (Fig. 12.9).
When microorganisms penetrate the ovarian tissue, purulent cavities (ovarian abscess) can form, and when they merge, the ovarian tissue melts. The ovary turns into a saccular formation filled with pus (pyovar; Fig. 12.10).

Rice. 12.8. Pyosalpinx. Laparoscopy

Rice. 12.9. Hydrosalpinx. Laparoscopy
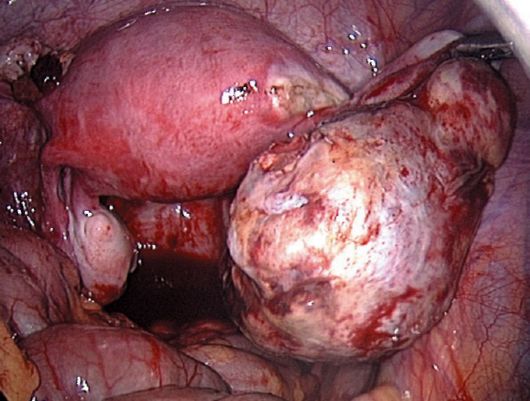
Rice. 12.10. Piovar. Laparoscopy
One form of complication of acute adnexitis is a tubo-ovarian abscess (Fig. 12.11), which occurs as a result of melting of the contacting walls of the pyovar and pyosalpinx.
Under certain conditions, through the fimbrial section of the tube, as well as as a result of rupture of the ovarian abscess, pyosalpinx, tubo-ovarian abscess, the infection can enter the abdominal cavity and cause inflammation of the pelvic peritoneum (pelvioperitonitis) (Fig. 12.12), and then other floors of the abdominal cavity (peritonitis) (Fig. 12.13) with the development of abscesses of the rectovaginal recess, interintestinal abscesses.
The disease most often occurs in women of the early reproductive period who are sexually active.
Clinical symptoms Acute salpingo-oophoritis (adnexitis) includes pain in the lower abdomen of varying intensity, increased body temperature to 38-40 ° C, chills, nausea, sometimes vomiting, purulent discharge from the genital tract, and dysuric phenomena. The severity of clinical symptoms is determined, on the one hand, by the virulence of the pathogens, and on the other, by the reactivity of the macroorganism.

Rice. 12.11. Tuboovarian abscess on the left. Laparoscopy

Rice. 12.12. Pelvioperitonitis. Laparoscopy

Rice. 12.13. Peritonitis. Laparoscopy
On general examination, the tongue is moist and covered with a white coating. Palpation of the abdomen may be painful in the hypogastric region. A gynecological examination reveals purulent or sanguineous-purulent discharge from the cervical canal, thickened, swollen, painful uterine appendages. When pyosalpinx, piovar, tubo-ovarian abscesses form in the area of the uterine appendages or posterior to the uterus, fixed, voluminous, painful formations without clear contours and uneven consistency can be identified, often forming a single conglomerate with the body of the uterus. In the peripheral blood, leukocytosis, a shift of the leukocyte formula to the left, an increase in ESR, the level of C-reactive protein, and dysproteinemia are detected. In urine analysis, increased protein content, leukocyturia, and bacteriuria are possible, which is associated with damage to the urethra and bladder. Sometimes the clinical picture of acute adnexitis is erased, but there are pronounced destructive changes in the uterine appendages.
Bacterioscopy of smears from the vagina and cervical canal reveals an increase in the number of leukocytes, coccal flora, gonococci, trichomonads, pseudomycelium and spores of a yeast-like fungus. Bacteriological examination of discharge from the cervical canal does not always reveal the causative agent of adnexitis. More accurate results are obtained by microbiological examination of the contents of the fallopian tubes and abdominal cavity, obtained during laparoscopy, laparotomy or puncture.
An ultrasound scan can visualize dilated fallopian tubes and free fluid in the pelvis (inflammatory exudate). The value of ultrasound increases with formed inflammatory tubo-ovarian formations (Fig. 12.14) of irregular shape, with unclear contours and heterogeneous echostructure. Free fluid in the pelvis most often indicates rupture of a purulent formation of the uterine appendages.
In the diagnosis of acute adnexitis, laparoscopy is the most informative. It allows you to determine the inflammatory process of the uterus and appendages, its severity and prevalence, to conduct a differential diagnosis of diseases accompanied by a picture of an “acute abdomen” to determine the correct tactics. In acute salpingitis, edematous, hyperemic fallopian tubes, the flow of serous-purulent or purulent exudate from the fimbrial sections (Fig. 12.15) and its accumulation in the rectovaginal cavity are revealed endoscopically. The ovaries may be enlarged as a result of secondary involvement in the inflammatory process. Pyosalpinx is visualized as a retort-shaped thickening of the tube in the ampullary section, the walls of the tube are thickened, swollen, compacted, the fimbrial section is sealed, and there is pus in the lumen. Pyovar looks like a voluminous formation of the ovary with a purulent cavity that has a dense capsule and a fibrin overlay. When a tubo-ovarian abscess forms, extensive adhesions form between the tube, ovary, uterus, intestinal loops, and pelvic wall. The long-term existence of a tubo-ovarian abscess leads to the formation of a dense capsule, delimiting

Rice. 12.14. Tuboovarian inflammatory formation. Ultrasound
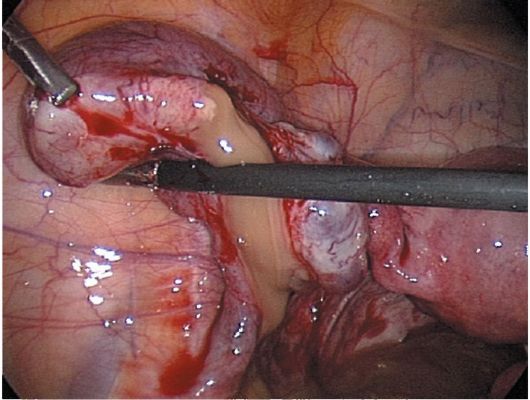
Rice. 12.15. Acute salpingitis. Laparoscopy
releasing the purulent cavity(s) from the surrounding tissues. When such purulent formations rupture, there is a perforation on their surface, from which pus enters the abdominal cavity (Fig. 12.16). The indicated changes in the internal genital organs, revealed during laparoscopy in the case of acute inflammation of the uterine appendages, can also be noted during transection performed to remove the source of inflammation. Obtaining purulent contents from space-occupying formations of the uterine appendages during their puncture through the posterior vaginal fornix under ultrasound control also indirectly confirms the inflammatory nature of the disease.

Rice. 12.16. Rupture of the right-sided pyosalpinx. Laparoscopy
Chronic salpingoophoritis (adnexitis) is a consequence of acute or subacute inflammation of the uterine appendages. The reasons for the chronicity of the inflammatory process include inadequate treatment of acute adnexitis, decreased reactivity of the body, and properties of the pathogen. Chronic salpingoophoritis is accompanied by the development of inflammatory infiltrates, connective tissue in the wall of the fallopian tubes and the formation of hydrosalpinxes. Dystrophic changes occur in the ovarian tissue; due to the narrowing of the lumen of blood vessels, microcirculation is disrupted, resulting in a decrease in the synthesis of sex steroid hormones. The consequence of acute or subacute inflammation of the uterine appendages is an adhesive process in the small pelvis between the tube, ovary, uterus, pelvic wall, bladder, omentum and intestinal loops (Fig. 12.17). The disease has a protracted course with periodic exacerbations.
Patients complain of dull, aching pain in the lower abdomen of varying intensity. Pain can radiate to the lower back, rectum, thigh, i.e. along the pelvic plexuses, and is accompanied by psycho-emotional (irritability, nervousness, insomnia, depression) and autonomic disorders. Pain intensifies after hypothermia, stress, menstruation. In addition, with chronic salpingoophoritis, menstrual dysfunction such as menometrorrhagia, opso- and oligomenorrhea, premenstrual syndrome caused by anovulation or insufficiency of the corpus luteum are observed. Infertility in chronic adnexitis is explained by both a violation of steroidogenesis in the ovaries and a tubo-peritoneal factor. Adhesions in the uterine appendages can cause ectopic pregnancy. Frequent exacerbations of the disease lead to sexual disorders - decreased libido, dyspareunia.
Exacerbations of chronic adnexitis occur due to an increase in the pathogenic properties of the pathogen, reinfection, and a decrease in the immunobiological properties of the macroorganism. With exacerbation, pain intensifies, general well-being is disturbed, body temperature may rise,

Rice. 12.17. Adhesive process in chronic adnexitis. Laparoscopy
There is purulent discharge from the genital tract. An objective examination reveals inflammatory changes in the uterine appendages of varying severity.
Diagnostics chronic salpingoophoritis can be extremely difficult, since chronic pelvic pain with periodic intensification occurs in other diseases (endometriosis, ovarian cysts and tumors, colitis, pelvic plexitis). Certain information allowing one to suspect chronic inflammation of the uterine appendages can be obtained from a bimanual examination of the pelvic organs, ultrasound of the pelvic organs, hysterosalpingography and GHA. During a gynecological examination, one can determine limited mobility of the uterine body (adhesions), the formation of an elongated shape in the area of the uterine appendages (hydrosalpinx). Ultrasound scanning is effective in diagnosing space-occupying formations of the uterine appendages. Hysterosalpingography and GHA help to identify adhesions in tubo-peritoneal factor infertility (accumulation of contrast agent in closed cavities). Currently, hysterosalpingography is used less and less due to the large number of diagnostic errors in the interpretation of x-rays.
With a long course of the disease with periodic pain in the lower abdomen, if antibiotic therapy is ineffective, you should resort to laparoscopy, which allows you to visually determine the presence or absence of signs of chronic adnexitis. These include adhesions in the pelvis and hydrosalpinx. The consequences of acute salpingoophoritis, most often of gonorrheal or chlamydial etiology, are considered to be adhesions between the surface of the liver and the diaphragm - Fitz-Hugh-Curtis syndrome (Fig. 12.18).
Pelvioperitonitis (inflammation of the pelvic peritoneum) occurs secondary to the penetration of pathogens from the uterus or its appendages into the pelvic cavity. Depending on the pathological contents in the pelvis, serous-fibrinous and purulent pelvioperitonitis are distinguished. The disease begins acutely, with the appearance of sharp pain in the lower abdomen,

Rice. 12.18. Fitz-Hugh-Curtis syndrome. Laparoscopy
an increase in body temperature to 39-40 °C, chills, nausea, vomiting, loose stools. During physical examination, a moist tongue coated with a white coating attracts attention. The abdomen is swollen, takes part in the act of breathing, and is painful on palpation in the lower parts; There, the Shchetkin-Blumberg symptom of peritoneal irritation is expressed to varying degrees, and tension in the anterior abdominal wall is noted. Palpation of the uterus and appendages during gynecological examination is difficult due to severe pain, the posterior vaginal vault is smoothed due to the accumulation of exudate in the rectovaginal cavity. Changes in clinical blood tests are characteristic of inflammation. Additional diagnostic methods include transvaginal ultrasound scanning, which helps clarify the condition of the uterus and appendages and determine free fluid (pus) in the pelvis. The most informative diagnostic method is laparoscopy: hyperemia of the pelvic peritoneum and adjacent intestinal loops with the presence of purulent contents in the rectovaginal cavity is visualized. As the acute phenomena subside as a result of the formation of adhesions of the uterus and appendages with the omentum, intestines, and bladder, inflammation is localized in the pelvic area. When puncturing the abdominal cavity through the posterior vaginal fornix, inflammatory exudate can be aspirated. A bacteriological analysis of the obtained material is carried out.
Parametritis- inflammation of the tissue surrounding the uterus. Occurs when infection spreads from the uterus after childbirth, abortion, curettage of the uterine mucosa, operations on the cervix, or when using an IUD. The infection penetrates the parametrial tissue through the lymphogenous route. Parametritis begins with the appearance of infiltration and the formation of serous inflammatory exudate at the site of the lesion. With a favorable course, the infiltrate and exudate resolve, but in some cases, fibrous connective tissue develops at the site of inflammation, which leads to a displacement of the uterus towards the lesion. When exudate suppurates, purulent parametritis occurs, which can be resolved by the release of pus into the rectum, less often into the bladder or abdominal cavity.
Clinical picture parametritis is caused by inflammation and intoxication: increased body temperature, headache, poor health, dry mouth, nausea, pain in the lower abdomen, radiating to the leg or lower back. Sometimes infiltration of the parametrium leads to compression of the ureter on the affected side, disruption of urine passage, and even the development of hydronephrosis. In the diagnosis of the disease, an important role is played by bimanual and rectovaginal examination, which determines the smoothness of the lateral vaginal vault, a dense, motionless, low-painful infiltrate of the parametrium at the site of the lesion, sometimes reaching the pelvic wall. Percussion over the superoanterior iliac spine on the side of the parametritis reveals dullness of percussion sound (Henter's symptom). In the blood, leukocytosis is observed with a shift in the leukocyte formula to the left, and an increase in ESR. Additional methods for diagnosing parametritis are pelvic ultrasound, CT and MRI.
When the parametrial tissue suppurates, the patient's condition sharply worsens - chills, hectic fever appear, and symptoms of intoxication intensify. If fibrous changes develop in the parametrium area, a dense cord is palpated, the uterus is displaced towards the affected side.
Gynecological peritonitis (diffuse damage to the peritoneum), along with sepsis, is the most severe form of manifestation of the inflammatory process of the internal genital organs and is characterized by the phenomena of severe endogenous intoxication and multiple organ failure, referred to as systemic inflammatory response syndrome.
In the development of peritonitis, it is customary to distinguish 3 stages: reactive, toxic and terminal. The reactive stage, which lasts about a day, is characterized by hyperemia, swelling of the peritoneum, exudation with the formation of fibrin, impaired vascular permeability with hemorrhagic manifestations of varying intensity, as well as signs of initial intoxication. Upon examination, patients are excited, complain of pain throughout the abdomen, increasing with changes in body position, increased body temperature, chills, nausea, and vomiting. On examination, the skin is pale with a gray tint, tachycardia is noted, the tongue is dry and coated. The abdomen is tense, palpation is sharply painful in all parts, symptoms of peritoneal irritation are positive, intestinal motility is slow. Blood tests reveal moderate leukocytosis with a shift to the left. In the toxic stage, which lasts about 2 days, symptoms of intoxication increase, and local manifestations of peritonitis become less pronounced. The condition of the patients is serious, they become lethargic and adynamic. Repeated vomiting and severe intestinal paresis lead to disturbances in water-electrolyte balance, acid-base status, and hypo- and dysproteinemia. Leukocytosis with a shift to the left increases. In the terminal stage, which occurs after 2-3 days, symptoms appear indicating deep damage to the central nervous system, the patients’ consciousness is confused, facial features are pointed, the skin is pale gray, cyanotic, with drops of sweat (Hippocrates’ face). Symptoms of multiple organ failure increase. The pulse becomes weak, arrhythmic, hypotension and bradycardia are observed, severe shortness of breath, oliguria, vomiting of stagnant contents, constipation is replaced by diarrhea.
Treatment of inflammatory diseases of the internal genital organs carried out in a hospital. The nature and intensity of complex therapy depend on the stage and severity of the inflammatory process, the type of pathogen, the immunobiological resistance of the macroorganism, etc. Creating mental and physical rest and following a diet with a predominance of easily digestible proteins and vitamins are important. An ice pack is placed on the hypogastric region.
Antibacterial therapy plays a central role. The drug is selected taking into account the spectrum and mechanism of action, pharmacokinetics, side effects, as well as the etiology of the disease. Due to the polymicrobial etiology of inflammation, drugs or combinations thereof should be used that are effective against most possible pathogens. For the purpose of treating acute inflammatory processes of the internal genitalia
organs use inhibitor-protected penicillin antibiotics (amoxicillin/clavulanate ♠, piperacillin/tazobactam, ampicillin/sulbactam), third generation cephalosporins (ceftriaxone, cefotaxime, cefoperazone, cefixime), fluoroquinolones (ciprofloxacin, ofloxacin, levofloxacin, moxifloc sacin), aminoglycosides (gentamicin, netyl -mycin, amikacin), lincosamines (lincomycin, clindamycin), macrolides (spiramycin, azithromycin, erythromycin), tetracyclines (doxycycline).
The possibility of the participation of gonococci and chlamydia in the acute inflammatory process of the internal genital organs suggests a combination of antibiotics that are effective against these microorganisms. It is advisable to combine antibiotics with nitroimidazole derivatives (metronidazole), which are highly active in the treatment of anaerobic infections. In case of severe inflammatory process, antibacterial drugs are started to be administered parenterally and continued for 24-48 hours after the onset of clinical improvement, and then prescribed orally. For complicated forms of the disease, carbapenem antibiotics can be used - imipenem or meropenem with the widest spectrum of antimicrobial activity. The total duration of antibacterial therapy is 7-14 days.
In order to prevent and treat possible fungal infections, it is recommended to include antimycotic drugs (fluconazole, ketoconazole, itraconazole) in the treatment complex. The patient should be strongly advised to refrain from unprotected sexual intercourse until she and her partner have completed a full course of treatment and examination.
In case of severe general reaction and intoxication, infusion therapy is prescribed for the purpose of detoxification, improving the rheological and coagulation properties of blood, eliminating hypovolemia, electrolyte disturbances (isotonic solutions of sodium chloride and glucose, Ringer's solution *, rheopolyglucin *, glucose-novocaine mixture, fraxiparine *, clexane *), restoration of the acid-base state (sodium bicarbonate solution), elimination of dysproteinemia (plasma, albumin solution). Infusion therapy, by reducing blood viscosity, improves the delivery of antibiotics to the site of inflammation and increases the effectiveness of antibacterial therapy.
Mandatory in the treatment of severe forms of inflammatory processes of the internal genital organs is the normalization of the function of the gastrointestinal tract.
In order to reduce sensitization to tissue breakdown products and microbial cell antigens, it is necessary to use antihistamines. Symptoms of inflammation (pain, swelling) are effectively reduced by NSAIDs (indomethacin, diclofenac - voltaren *, ibuprofen, piroxicam). To correct impaired immunity and increase nonspecific resistance of the body, γ-globulin, levamisole, T-activin, thymalin ♠, thymogen ♠, α-interferon, interferon, stimulators of the synthesis of endogenous interferon (cycloferon ♠, neovir ♠, tiloron-amiksin ♠) should be used ) etc.), ascorbic acid, vitamins E, group B, adaptogens.
In difficult situations, to restore disturbed homeostasis, they resort to efferent (extracorporeal) methods of treatment - plasma
mapheresis, hemosorption, peritoneal dialysis, ultrahemofiltration. Regardless of the etiology of inflammation, reinfusion of blood irradiated with UV rays is extremely effective. The procedure has a multifaceted effect: eliminates hemorheological and coagulation disorders, promotes saturation of hemoglobin with oxygen, detoxification of the body, activates the immune system, and provides a bactericidal and virocidal effect.
In the acute phase of the inflammatory process, physiotherapy can be prescribed - UHF currents to the hypogastric region, subsequently, when signs of inflammation subside, - electrophoresis of potassium iodide, copper, zinc, magnesium, phonophoresis of hydrocortisone, exposure to an alternating electromagnetic field, laser therapy.
When treating endometritis, it is advisable to perform hysteroscopy with washing the uterine cavity with antiseptic solutions, removing, if necessary, the remains of the fertilized egg, placental tissue, and foreign bodies.
The effectiveness of conservative therapy is assessed after 12-24 hours. The lack of effect in patients with pelvioperitonitis during this period, the increase in local and general symptoms of inflammation, and the inability to exclude rupture of a purulent tubo-ovarian formation are indications for surgical treatment.
For pyosalpinxes and pyovars, puncture of purulent formations can be performed through the posterior vaginal fornix under ultrasound scanning control. During puncture, aspiration of the contents is carried out, followed by bacteriological examination and washing of purulent cavities with antiseptics or antibiotic solutions. This tactic allows you to eliminate acute symptoms of the inflammatory process and, if necessary, perform organ-preserving operations in the future.
The best results in the treatment of acute inflammatory diseases of the uterine appendages are obtained by laparoscopy. The value of the latter, in addition to assessing the severity and prevalence of the inflammatory process, lies in the ability to lyse adhesions, open or remove purulent tubo-ovarian formations, perform targeted drainage and sanitation of the abdominal cavity, carry out intra-abdominal perfusion and infusion of various medicinal solutions. To preserve reproductive function, dynamic laparoscopy is advisable (Fig. 12.19), during which various therapeutic manipulations are performed: separation of adhesions, aspiration of pathological effusion, washing of the abdominal cavity with antiseptics. Dynamic laparoscopy increases the effectiveness of anti-inflammatory therapy and prevents the formation of adhesions, which is especially important for patients planning pregnancy.
Transsection (lower median laparotomy) is indicated for rupture of a purulent tubo-ovarian formation, peritonitis, intra-abdominal abscesses, failure of treatment within 24 hours after drainage of the abdominal cavity using a laparoscope, and if it is impossible to perform laparoscopy. Laparotomy access is also used in patients with purulent tubo-ovarian formations in pre- and postmenopause, if it is necessary to remove the uterus.

Rice. 12.19. Pyosalpinx on the 2nd day after opening. Laparoscopy
The extent of the operation is determined by the patient’s age, the degree of destructive changes and the prevalence of the inflammatory process, and concomitant pathology. Extirpation of the uterus with appendages on one or both sides is carried out if the uterus is the source of the inflammatory process (endomyometritis, panmetritis when using an IUD, after childbirth, abortion and other intrauterine interventions), there are concomitant lesions of the body and cervix, with diffuse peritonitis, multiple abscesses in abdominal cavity. In patients of reproductive age, one should strive to perform organ-conserving operations or, as a last resort, to preserve ovarian tissue. The surgical intervention is completed with drainage of the abdominal cavity.
In a patient with acute inflammatory disease of the genital organs, it is necessary to identify sexual partners and offer them to undergo examination for gonorrhea and chlamydia.
Treatment of chronic inflammatory diseases of the internal genital organs includes the elimination of pain, normalization of menstrual and reproductive functions.
Treatment of exacerbations of chronic inflammation of the uterine appendages is carried out in a antenatal clinic or in a hospital according to the same principles as the treatment of acute inflammation.
The main role in the treatment of chronic inflammatory diseases of the internal genital organs outside of exacerbations belongs to physiotherapy. Drug therapy is aimed at increasing the immunobiological resistance of the body, eliminating residual effects of the inflammatory process, and pain. NSAIDs are used (administered mainly rectally), vitamins, antioxidants, immunostimulants, stimulators of endogenous interferon synthesis. At the same time, correction of menstrual irregularities is carried out, including with the help of hormonal drugs.
Restoration of reproductive function is possible after laparoscopic separation of adhesions, fimbryoplasty, and salpingostomy, which are performed in patients under 35 years of age. If operational
In vitro fertilization (IVF) is indicated for the treatment of tubo-peritoneal infertility.
Gonorrhea
Gonorrhea- infectious disease caused by gonococcus (Neisseria gonorrhoeae), with predominant damage to the genitourinary organs. The disease is diagnosed in 200 million people every year. Past gonorrhea often becomes the cause of both female and male infertility.
Etiology and pathogenesis. Gonococcus is a paired bean-shaped coccus (diplococcus) that is not Gram stained; is necessarily located intracellularly (in the cytoplasm of leukocytes). Gonococci are highly sensitive to environmental factors: they die at temperatures above 55 °C, when dried, treated with antiseptic solutions, or under the influence of direct sunlight. Gonococcus remains viable in fresh pus until dry. In this regard, infection occurs mainly through sexual contact (from an infected partner). The contagiousness of the infection for women is 50-70%, for men - 25-50%. Infection through household means (through dirty linen, towels, washcloths) is much less common, mainly in girls. The possibility of intrauterine infection remains controversial. Gonococcus is immobile, does not form spores, and is attached to the surface of epithelial cells, sperm, and erythrocytes by means of thin tubular filaments (pili). Outside, gonococci are covered with a capsule-like substance that makes them difficult to digest. The pathogen can survive inside leukocytes, trichomonads, epithelial cells (incomplete phagocytosis), which complicates treatment. With inadequate treatment, L-forms can be formed, which are insensitive to the drugs that caused their formation, antibodies and complement as a result of the loss of some antigenic properties. The persistence of L-forms complicates diagnosis and treatment and contributes to the survival of the infection in the body. Due to the widespread use of antibiotics, many strains of gonococcus have appeared that produce the β-lactamase enzyme and, accordingly, are resistant to antibiotics containing a β-lactam ring.
Gonococci primarily affect parts of the genitourinary system lined with columnar epithelium - the mucous membrane of the cervical canal, fallopian tubes, urethra, paraurethral and large vestibular glands. With genital-oral contacts, gonorrheal pharyngitis, tonsillitis and stomatitis can develop, with genital-anal contacts - gonorrheal proctitis. When an infection enters the mucous membrane of the eyes, including when the fetus passes through the infected birth canal, signs of gonorrheal conjunctivitis appear.
The vaginal wall, covered with stratified squamous epithelium, is resistant to gonococcal infection. However, if the epithelium becomes thinner or becomes loose, gonorrheal vaginitis may develop (during pregnancy, in girls, in postmenopausal women).
Gonococci quickly fix on the surface of epithelial cells with the help of pili, and then penetrate deep into the cells, intercellular spaces and subepithelial space, causing destruction of the epithelium and an inflammatory reaction.
Gonorrheal infection spreads more often along the length (canalicularly) from the lower parts of the genitourinary tract to the upper ones. Advancement is often facilitated by the adhesion of gonococcus to the surface of sperm and enterobiasis inside Trichomonas, which are active carriers of infection.
Sometimes gonococci enter the bloodstream (usually they die due to the bactericidal properties of the serum), leading to generalization of the infection and the appearance of extragenital lesions, primarily joints. Gonorrheal endocarditis and meningitis develop less frequently.
In response to the introduction of gonorrhea infection, the body produces antibodies, but immunity does not develop. A person can become infected and suffer from gonorrhea many times; this is explained by the antigenic variability of gonococcus. The incubation period of gonorrhea ranges from 3 to 15 days, less often - up to 1 month.
There are the following types of gonorrheal infection: gonorrhea of the lower genitourinary system, upper genitourinary system and pelvic organs, and gonorrhea of other organs. Gonorrhea of the lower parts of the genitourinary system includes damage to the urethra, paraurethral glands, glands of the vestibule of the vagina, mucous membrane of the cervical canal, vagina; gonorrhea of the upper parts of the genitourinary system (ascending) includes damage to the uterus, appendages and peritoneum.
Fresh gonorrhea is also distinguished (duration up to 2 months), which is divided into acute, subacute, torpid (low-symptomatic or asymptomatic with scanty exudate in which gonococci are found), and chronic (lasting more than 2 months or of unknown duration). Chronic gonorrhea can occur with exacerbations. Gonococcal carriage is possible when the pathogen does not cause the appearance of exudate and there are no subjective disorders.
Clinical manifestations. Gonorrhea of the lower genitourinary system is often asymptomatic. Severe manifestations of the disease include symptoms of dysuria, itching and burning in the vagina, purulent, creamy discharge from the cervical canal. On examination, hyperemia and swelling of the urethral orifice and cervical canal are detected.
Upper gonorrhea (ascending) usually causes a disturbance in the general condition, complaints of pain in the lower abdomen, an increase in body temperature up to 39 ° C, nausea, sometimes vomiting, chills, loose stools, frequent and painful urination, and menstrual irregularities. The spread of infection beyond the internal os is facilitated by artificial interventions - abortion, curettage of the uterine mucosa, probing of the uterine cavity, taking endometrial aspirate, cervical biopsy, insertion of an IUD. An acute ascending inflammatory process is often preceded by menstruation and childbirth. An objective examination reveals purulent or sanguineous-purulent discharge from the cervical
canal, enlarged, painful, soft consistency uterus (with endomyometritis), swollen painful appendages (with salpingo-oophoritis), pain on palpation of the abdomen, symptoms of peritoneal irritation (with peritonitis). An acute inflammatory process in the uterine appendages is complicated by the development of tubo-ovarian inflammatory formations up to the occurrence of abscesses (especially in women using
VMC).
Currently, the gonorrheal process does not have typical clinical signs, since in almost all cases a mixed infection is detected. Mixed infection lengthens the incubation period, promotes more frequent recurrence, and complicates diagnosis and treatment.
Chronicity of the inflammatory process leads to disruption of the menstrual cycle, the development of adhesions in the pelvis, which can lead to infertility, ectopic pregnancy, miscarriage, and chronic pelvic pain syndrome.
The main methods of laboratory diagnosis of gonorrhea are bacterioscopic and bacteriological, aimed at identifying the pathogen. During bacterioscopic examination, gonococci are identified by pairing, intracellular location and gram-negativity (Fig. 12.20). Due to the high variability under the influence of the environment, gonococcus cannot always be detected by bacterioscopy. To identify erased and asymptomatic forms of gonorrhea, as well as infections in children and pregnant women, the bacteriological method is more suitable. The material is inoculated on artificial nutrient media. If the material is contaminated with foreign accompanying flora, the isolation of gonococcus becomes difficult, so selective media with the addition of antibiotics are used. If it is impossible to inoculate immediately, the material for research is placed in a transport medium. Cultures grown on a nutrient medium are subjected to microscopy, their properties and sensitivity to antibiotics are determined. Material for microscopy and culture is taken from the cervical canal, vagina, and urethra.

Rice. 12.20. Microscopy of a vaginal smear. Gonococcus inside neutrophils
Treatment. Sexual partners are subject to treatment if gonococci are detected by bacterioscopic or cultural methods. The main focus is on antibiotic therapy, and the growth of gonococcus strains resistant to modern antibiotics should be taken into account. The reason for the ineffectiveness of treatment may be the ability of gonococcus to form L-forms, produce β-lactamase, and persist inside cells. Treatment is prescribed taking into account the form of the disease, localization of the inflammatory process, complications, concomitant infection, and sensitivity of the pathogen to antibiotics.
Etiotropic treatment of fresh gonorrhea of the lower parts of the genitourinary system without complications consists of a single use of one of the antibiotics: ceftriaxone, azithromycin, ciprofloxacin, spectinomycin, ofloxacin, amoxiclav ♠, cefixime. For the treatment of gonorrhea of the lower parts of the genitourinary system with complications and gonorrhea of the upper parts and pelvic organs, it is proposed to use the same antibiotics for 7 days.
During treatment, avoid alcohol and sexual intercourse. During the follow-up period, it is strongly recommended to use a condom. In case of mixed infection, you should choose the drug, dose and duration of its use, taking into account the isolated microflora. After completion of treatment with antibacterial drugs, it is advisable to prescribe eubiotics intravaginally (vagilak ♠, lactobacterin ♠, bifidum-bacterin ♠, acylact ♠).
Treatment of gonorrhea in children is reduced to the administration of ceftriaxone or spectinomycin once.
For fresh acute gonorrhea of the lower parts of the genitourinary system, etiotropic treatment is sufficient. In the case of a torpid or chronic course of the disease in the absence of symptoms, antibiotic treatment is recommended to be supplemented with immunotherapy and physiotherapy.
Immunotherapy for gonorrhea is divided into specific (gonovaccine *) and nonspecific (pyrogenal ♠, prodigiosan ♠, autohemotherapy). Immunotherapy is carried out after the acute phenomena have subsided against the background of ongoing antibiotic therapy or before the start of antibiotic treatment (in subacute, torpid or chronic course). Immunotherapy is not indicated for children under 3 years of age. In general, the use of immunomodulatory drugs for gonorrhea is currently limited and should be strictly justified.
The principles of treatment of acute forms of ascending gonorrhea are similar to those in the treatment of inflammatory diseases of the internal genital organs.
Cure criteria gonorrhea (7-10 days after the end of therapy) is the disappearance of symptoms of the disease and the elimination of gonococci from the urethra, cervical canal and rectum according to bacterioscopy. It is possible to carry out a combined provocation, in which smears are taken after 24, 48 and 72 hours and the secretions are cultured after 2 or 3 days. Provocation is divided into physiological (menstruation), chemical (lubrication of the urethra with a 1-2% solution of silver nitrate, the cervical canal - with a 2-5% solution), biological (intramuscular
administration of gonovaccin* in a dose of 500 million microbial bodies), physical (inductothermy), nutritional (spicy, salty foods, alcohol). Combined provocation combines all types of provocation.
The second control study is carried out on the days of the next menstruation. It consists of bacterioscopy of discharge from the urethra, cervical canal and rectum, taken 3 times with an interval of 24 hours.
During the third control examination (after the end of menstruation), a combined provocation is performed, after which a bacterioscopic (after 24, 48 and 72 hours) and bacteriological (after 2 or 3 days) examination is performed. If gonococci are absent, the patient is removed from the register.
If the source of infection is unknown, it is advisable to carry out serological tests for syphilis, HIV, hepatitis B and C (before treatment and 3 months after its completion).
Many experts dispute the advisability of provocations and multiple control examinations and propose reducing the period of observation of women after full treatment of gonococcal infection, since with the high effectiveness of modern drugs, the clinical and economic meaning of routine measures is lost. It is recommended to have at least one follow-up examination after completion of treatment to determine the adequacy of therapy, the absence of gonorrhea symptoms, and to identify partners. Laboratory control is carried out only in case of ongoing disease, if there is a possibility of re-infection or resistance of the pathogen.
Sexual partners are involved in examination and treatment if sexual contact occurred 30 days before the onset of symptoms of the disease, as well as persons who were in close household contact with the patient. For asymptomatic gonorrhea, sexual partners who had contact within 60 days before diagnosis are examined. Children of mothers with gonorrhea are subject to examination, as well as girls in case of detection of gonorrhea in persons caring for them.
Prevention consists of timely identification and adequate treatment of patients with gonorrhea. For this purpose, preventive examinations are carried out, especially for workers in child care institutions and canteens. Pregnant women registered at the antenatal clinic or applying for an abortion are subject to mandatory examination. Personal prevention comes down to maintaining personal hygiene, avoiding casual sex, and using a condom. Prevention of gonorrhea in newborns is carried out immediately after birth: 1-2 drops of a 30% solution of sulfacetamide (sodium sulfacyl *) are instilled into the conjunctival sac.
Urogenital chlamydia
Urogenital chlamydia - one of the most common sexually transmitted infections. The number of people infected with chlamydia is steadily increasing; Every year, 90 million cases of the disease are registered worldwide. The widespread prevalence of chlamydia is due to the erasure of clinical
symptoms, the complexity of diagnosis, the emergence of antibiotic-resistant strains, as well as social factors: an increase in the frequency of extramarital sex, prostitution, etc. Chlamydia is often the cause of non-gonococcal urethritis, infertility, pelvic inflammatory diseases, pneumonia and conjunctivitis in newborns.
Chlamydia is unstable in the external environment and easily dies when exposed to antiseptics, ultraviolet rays, boiling, and drying.
Infection occurs mainly through sexual contact with an infected partner, transplacentally and intranatally, rarely through household contact.
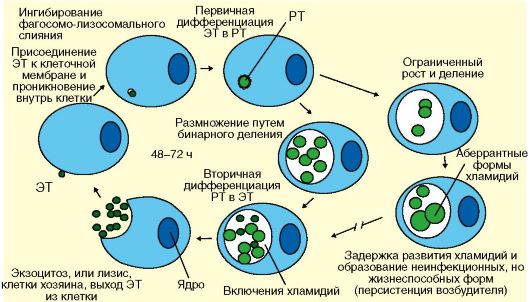
Rice. 12.21. Life cycle of chlamydia: ET - elementary bodies; RT - reticular bodies
through toilet items, linen, shared bed. The causative agent of the disease exhibits a high affinity for columnar epithelial cells (endocervix, endosalpinx, urethra). In addition, chlamydia, absorbed by monocytes, spreads through the bloodstream and settles in tissues (joints, heart, lungs, etc.), causing multifocal lesions. The main pathogenetic link of chlamydia is the development of a scar-adhesive process in the affected tissues as a consequence of the inflammatory reaction.
Chlamydial infection causes pronounced changes in both cellular and humoral immunity. One should take into account the ability of chlamydia, under the influence of inadequate therapy, to transform into L-forms and (or) change its antigenic structure, which complicates the diagnosis and treatment of the disease.
Classification. There are fresh (disease duration up to 2 months) and chronic (disease duration more than 2 months) chlamydia; cases of carriage of chlamydial infection have been reported. In addition, the disease is divided into chlamydia of the lower parts of the genitourinary system, its upper parts and pelvic organs, and chlamydia of other localizations.
Clinical symptoms. The incubation period for chlamydia ranges from 5 to 30 days, averaging 2-3 weeks. Urogenital chlamydia is characterized by polymorphism of clinical manifestations, absence of specific signs, asymptomatic or asymptomatic long-term course, and a tendency to relapse. Acute forms of the disease have been observed in mixed infections.
Most often, chlamydial infection affects the mucous membrane of the cervical canal. Chlamydial cervicitis often remains asymptomatic. Sometimes patients note the appearance of serous-purulent discharge from the genital tract, and when urethritis occurs, itching in the urethral area, painful and frequent urination, purulent discharge from the urethra in the morning (the “morning drop” symptom).
Ascending urogenital chlamydial infection determines the development of salpingo-oophoritis, pelvioperitonitis, peritonitis, which do not have specific symptoms, except for a protracted “erased” course during the chronicization of the inflammatory process. The consequences of chlamydia infection of the pelvic organs include adhesions in the area of the uterine appendages, infertility, and ectopic pregnancy.
Extragenital chlamydia includes Reiter's disease, which includes the triad: arthritis, conjunctivitis, urethritis.
Chlamydia in newborns manifests itself as vulvovaginitis, urethritis, conjunctivitis, and pneumonia.
Due to scanty and (or) nonspecific symptoms, it is impossible to recognize the disease based on the clinical picture. The diagnosis of chlamydia is made only based on the results of laboratory research methods. Laboratory diagnosis of chlamydia involves identifying the pathogen itself or its antigens. The material for the study is scrapings from the cervical canal, urethra, and conjunctiva. Microscopy of smears stained according to Romanovsky-Giemsa allows identifying the pathogen in 25-30% of cases. In this case, the elementary bodies are stained red
In order to clarify the diagnosis and determine the phase of the disease, the detection of chlamydial antibodies of classes A, M, G in blood serum is used. In the acute phase of chlamydial infection, the IgM titer increases; during the transition to the chronic phase, the IgA and then IgG titers increase. A decrease in titers of chlamydial antibodies of classes A and G during treatment serves as an indicator of its effectiveness.
Treatment. All sexual partners are subject to mandatory examination and, if necessary, treatment. During the period of treatment and follow-up, you should abstain from sexual intercourse or use a condom.
For uncomplicated chlamydia of the genitourinary organs, one of the antibiotics is recommended: azithromycin, roxithromycin, spiramycin, josamycin, doxycycline, ofloxacin, erythromycin for 7-10 days.
For chlamydia of the pelvic organs, the same drugs are used, but for at least 14-21 days. It is preferable to prescribe azithromycin - 1.0 g orally once a week for 3 weeks.
Newborns and children weighing up to 45 kg are prescribed erythromycin for 10-14 days. For children under 8 years of age weighing more than 45 kg and over 8 years of age, erythromycin and azithromycin are used according to adult treatment regimens.
Due to the decrease in immune and interferon status in chlamydia, along with etiotropic treatment, it is advisable to include interferon preparations (viferon ♠, reaferon ♠, kipferon ♠) or inducers of endogenous interferon synthesis (cycloferon *, neovir *, sodium ribonucleate - ridostin ♠, tiloron) . In addition, antioxidants, vitamins, physiotherapy are prescribed, and vaginal microbiocenosis is corrected with eubiotics.
The criteria for cure are the resolution of clinical manifestations and eradication Chlamydia trachomatis according to laboratory tests carried out after 7-10 days, and then after 3-4 weeks.
Prevention urogenital chlamydia is to identify and timely treat patients and exclude casual sexual contacts.
Genital herpes
Herpes is one of the most common human viral infections. Herpes simplex virus (HSV) infection rate is 90%; 20% of the world's population have clinical manifestations of in-
infections. Genital herpes is a sexually transmitted chronic recurrent viral disease.
Etiology and pathogenesis. The causative agent of the disease is the herpes simplex virus serotypes HSV-1 and HSV-2 (more often HSV-2). The herpes virus is quite large, contains DNA, is unstable in the external environment and quickly dies when dried, heated, or exposed to disinfectant solutions.
Infection occurs through sexual contact from infected partners who are not always aware of their infection. Recently, the oral-genital route of infection has become of great epidemiological importance. Contagiousness for women reaches 90%. The household route of transmission of infection (through toilet items, underwear) is unlikely, although it cannot be ruled out. Herpetic infection can be transmitted from a sick mother to the fetus transplacentally and intranatally.
The virus enters the body through damaged mucous membranes of the genitals, urethra, rectum and skin. Blistering rashes appear at the injection site. HSV, entering the bloodstream and lymphatic system, can settle in internal organs and the nervous system. The virus can also penetrate through the nerve endings of the skin and mucous membranes into the ganglia of the peripheral and central nervous system, where it persists for life. Periodically migrating between ganglia (in genital herpes these are the ganglia of the lumbar and sacral sympathetic chain) and the surface of the skin, the virus causes clinical signs of relapse of the disease. The manifestation of herpes infection is facilitated by a decrease in immunoreactivity, hypothermia or overheating, chronic diseases, menstruation, surgical interventions, physical or mental trauma, and alcohol intake. HSV, having neurodermotropism, affects the skin and mucous membranes (face, genitals), the central nervous system (meningitis, encephalitis) and the peripheral nervous system (gangliolitis), eyes (keratitis, conjunctivitis).
Classification. Clinically, the first episode of the disease and relapses of genital herpes are distinguished, as well as the typical course of the infection (with herpetic rashes), atypical (without rashes) and viral carriage.
Clinical symptoms. The incubation period is 3-9 days. The first episode of the disease is more violent than subsequent relapses. After a short prodromal period with local itching and hyperesthesia, the clinical picture develops. The typical course of genital herpes is accompanied by extragenital symptoms (viremia, intoxication) and genital signs (local manifestations of the disease). Extragenital symptoms include headache, fever, chills, myalgia, nausea, and malaise. Usually these symptoms disappear with the appearance of blistering rashes on the perineum, skin of the external genitalia, in the vagina, on the cervix (genital signs). Vesicles (2-3 mm in size) are surrounded by an area of hyperemic, edematous mucous membrane. After 2-3 days of existence, they open with the formation of ulcers covered with a grayish-yellow
purulent (due to secondary infection) plaque. Patients complain of pain, itching, burning at the site of the lesion, heaviness in the lower abdomen, and dysuria. With severe manifestations of the disease, low-grade fever, headache, and enlarged peripheral lymph nodes are noted. The acute period of herpetic infection lasts 8-10 days, after which visible manifestations of the disease disappear.
Currently, the frequency of atypical forms of genital herpes has reached 40-75%. These forms of the disease are erased, without herpetic eruptions, and are accompanied by damage not only to the skin and mucous membranes, but also to the internal genital organs. There are complaints of itching, burning in the affected area, leucorrhoea that does not respond to antibiotic therapy, recurrent erosions and leukoplakia of the cervix, recurrent miscarriage, and infertility. Herpes of the upper genital tract is characterized by symptoms of nonspecific inflammation. Patients are bothered by periodic pain in the lower abdomen; conventional therapy does not give the desired effect.
In all forms of the disease, the nervous system suffers, which manifests itself in neuropsychic disorders - drowsiness, irritability, poor sleep, depressed mood, decreased performance.
The frequency of relapses depends on the immunobiological resistance of the macroorganism and ranges from once every 2-3 years to once every month.
Diagnosis of genital herpes is based on medical history, complaints, and the results of an objective examination. Recognizing typical forms of the disease is usually not difficult, since the vesicular rash has characteristic signs. However, it is necessary to distinguish ulcers after opening of herpetic vesicles from syphilitic ulcers - dense, painless, with smooth edges. Diagnosis of atypical forms of genital herpes is extremely difficult.
Highly sensitive and specific laboratory diagnostic methods are used: cultivating the virus on a chicken embryo cell culture (gold standard) or identifying the viral antigen using ELISA methods; immunofluorescent method using PCR. The material for the study is discharge from herpetic vesicles, vagina, cervical canal, and urethra. A simple determination of antibodies in blood serum to the virus is not an accurate diagnostic criterion, since it only reflects HSV infection, including not only genital infection. A diagnosis made only on the basis of serological tests may be erroneous.
Treatment. Sexual partners of a patient with genital herpes are tested for HSV and treated if there are clinical signs of infection. Until the symptoms of the disease disappear, it is recommended to abstain from sexual intercourse or use condoms.
Since there are currently no methods for eliminating HSV from the body, the goal of treatment is to suppress the replication of the virus during the period of exacerbation of the disease and the formation of stable immunity to prevent relapses of herpes infection.
For the treatment of the first clinical episode and in case of relapse of genital herpes, antiviral drugs (acyclovir, valaclovir) are recommended for 5-10 days.
An integrated approach involves the use of nonspecific (T-activin, thymalin ♠, thymogen ♠, inosine pranobex - groprinosin ♠), myelopid * according to standard regimens and specific (antiherpetic γ-globulin, herpetic vaccine) immunotherapy. An extremely important link in the treatment of herpes is the correction of disturbances in the interferon system as the main barrier to the introduction of a viral infection into the body. Inducers of endogenous interferon synthesis have a good effect: Poludanum ♠, Cycloferon ♠, Neovir ♠, Tiloron. Interferon preparations are used as replacement therapy - Viferon ♠, Kipferon ♠ in rectal suppositories, Reaferon ♠ intramuscularly, etc.
To prevent relapses, a herpetic vaccine, interferonogens, as well as antiviral and immune drugs are used. The duration of therapy is determined individually.
The criteria for the effectiveness of treatment are the disappearance of clinical manifestations of the disease (relapse) and positive dynamics in the titer of specific antibodies.
Genital tuberculosis
Tuberculosis- an infectious disease caused by mycobacterium (Koch bacterium). Genital tuberculosis, as a rule, it develops secondarily, as a result of the transfer of infection from the primary lesion (usually from the lungs, less often from the intestines). Despite the progress of medicine, the incidence of tuberculosis in the world is increasing, especially in countries with low living standards. Damage to the genitourinary organs ranks first among extrapulmonary forms of tuberculosis. It is likely that genital tuberculosis affects the genital organs much more often than is recorded, since lifetime diagnosis does not exceed 6.5%.
Etiology and pathogenesis. From the primary focus, when the body’s immune resistance decreases (chronic infections, stress, malnutrition, etc.), mycobacteria enter the genitals. The infection spreads mainly by hematogenous route, most often with primary dissemination in childhood or puberty. With tuberculous lesions of the peritoneum, the pathogen enters the fallopian tubes lymphogenously or by contact. Direct infection through sexual contact with a patient with genital tuberculosis is only theoretically possible, since the stratified squamous epithelium of the vulva, vagina and vaginal portion of the cervix is resistant to mycobacteria.
In the structure of genital tuberculosis, the first place in frequency is occupied by damage to the fallopian tubes, the second - by the endometrium. Tuberculosis of the ovaries and cervix is less common, and tuberculosis of the vagina and external genitalia is extremely rare.
In the lesions, morphohistological changes typical of tuberculosis develop: exudation and proliferation of tissue elements, caseous necrosis. Tuberculosis of the fallopian tubes often ends with their obliteration, exudative-proliferative processes can lead to the formation of pyosalpinx, and when the muscular layer of the fallopian tubes is involved in a specific proliferative process, tubercles (tubercles) are formed in it, which is called nodous inflammation. With tuberculous endometritis, productive changes also predominate - tuberculous tubercles, caseous necrosis of individual areas. Tuberculosis of the uterine appendages is often accompanied by involvement of the peritoneum with ascites, intestinal loops with the formation of adhesions, and in some cases fistulas. Genital tuberculosis is often combined with damage to the urinary tract.
Classification. In accordance with the clinical and morphological classification, there are:
Chronic forms - with productive changes and mildly expressed clinical symptoms;
Subacute form - with exudative-proliferative changes and significant lesions;
Caseous form - with severe and acute processes;
Completed tuberculosis process - with encapsulation of known foci.
Clinical picture. The first symptoms of the disease may appear already during puberty, but mostly women aged 20-30 suffer from genital tuberculosis. In rare cases, the disease occurs in older or postmenopausal patients.
Genital tuberculosis has a mostly blurred clinical picture with a wide variety of symptoms, which is explained by the variability of pathological changes. A decrease in generative function (infertility) is the main, and sometimes the only, symptom of the disease. The causes of infertility, often primary, include endocrine disorders, lesions of the fallopian tubes and endometrium. In more than half of the patients, menstrual function is disrupted: amenorrhea (primary and secondary), oligomenorrhea, irregular menstruation, algomenorrhea, and less commonly menorrhagia and metrorrhagia occur. Menstrual dysfunction is associated with damage to the ovarian parenchyma, endometrium, as well as tuberculosis intoxication. A chronic disease with a predominance of exudation causes low-grade fever and nagging, aching pain in the lower abdomen due to adhesions in the pelvis, damage to nerve endings, vascular sclerosis and hypoxia of the tissues of the internal genital organs. Other manifestations of the disease include signs of tuberculosis intoxication (weakness, periodic fever, night sweats, decreased appetite, weight loss) associated with the development of exudative or caseous changes in the internal genital organs.
In young patients, genital tuberculosis can begin with signs of an “acute abdomen,” which often leads to surgical interventions due to suspected acute appendicitis, ectopic pregnancy, or ovarian apoplexy.
Due to the absence of pathognomonic symptoms and the blurred clinical symptoms, the diagnosis of genital tuberculosis is difficult. The idea of a tuberculosis etiology of the disease can be suggested by a correctly and carefully collected anamnesis with indications of the patient’s contact with a patient with tuberculosis, past pneumonia, pleurisy, observation in an anti-tuberculosis dispensary, the presence of extragenital foci of tuberculosis in the body, as well as the occurrence of an inflammatory process in the uterine appendages in young patients who were not sexually active, especially in combination with amenorrhea, and prolonged low-grade fever. A gynecological examination sometimes reveals acute, subacute or chronic inflammatory damage to the uterine appendages, most pronounced when proliferative or caseous processes predominate, signs of adhesions in the pelvis with displacement of the uterus. Gynecological examination findings are usually nonspecific.
To clarify the diagnosis, a tuberculin test (Koch test) is used. Tuberculin* is administered subcutaneously at a dose of 20 or 50 TU, after which the general and focal reactions are assessed. The general reaction is manifested by an increase in body temperature (more than 0.5 °C), including in the cervical area (cervical electrothermometry), increased heart rate (more than 100 per minute), an increase in the number of band neutrophils, monocytes, a change in the number of lymphocytes, an increase ESR. A general reaction occurs regardless of the location of the tuberculosis lesion, while a focal reaction occurs in its zone. A focal reaction is expressed in the appearance or intensification of pain in the lower abdomen, swelling and pain on palpation of the uterine appendages. Tuberculin tests are contraindicated in active tuberculosis, diabetes mellitus, severe liver and kidney dysfunction.
Microbiological methods remain the most accurate methods for diagnosing genital tuberculosis, which make it possible to detect mycobacteria in tissues. Discharge from the genital tract, menstrual blood, endometrial scrapings or washings from the uterine cavity, the contents of inflammatory foci, etc. are examined. The material is inoculated on special artificial nutrient media at least three times. However, the inoculation rate of mycobacteria is low, which is explained by the peculiarities of the tuberculosis process. A highly sensitive and specific method for identifying the pathogen is PCR, which allows you to determine DNA sections characteristic of Mycobacterium tuberculosis. However, the research material may contain PCR inhibitors, which leads to false negative results.
Laparoscopy makes it possible to identify specific changes in the pelvic organs - adhesions, tuberculous tubercles on the visceral peritoneum covering the uterus, tubes, caseous foci in combination with inflammatory changes in the appendages. In addition, during laparoscopy, it is possible to take material for bacteriological and histological examination, and also, if necessary, carry out surgical correction: lysis of adhesions, restoration of patency of the fallopian tubes, etc.
Histological examination of tissues obtained through biopsy, separate diagnostic curettage (it is better to carry it out 2-3 days in advance)
before menstruation), reveals signs of tuberculosis. A cytological method is also used to study aspirate from the uterine cavity and smears from the cervix, which makes it possible to detect Langhans giant cells specific for tuberculosis.
Diagnosis of genital tuberculosis helps hysterosalpingography. Radiographs reveal signs characteristic of tuberculous lesions of the genital organs: displacement of the uterine body due to adhesions, intrauterine synechiae, obliteration of the uterine cavity (Asherman's syndrome), uneven contours of the tubes with closed fimbrial sections, expansion of the distal parts of the tubes in the form of an onion, distinct changes in the tubes , cystic dilatations or diverticula, tubal rigidity (lack of peristalsis), calcifications. Plain radiographs of the pelvic organs reveal pathological shadows - calcifications in the tubes, ovaries, lymph nodes, foci of caseous decay. To avoid exacerbation of the tuberculosis process, hysterosalpingography is performed in the absence of signs of acute and subacute inflammation.
Diagnosis is complemented by ultrasound scanning of the pelvic organs. However, interpretation of the data obtained is very difficult and is only accessible to a specialist in the field of genital tuberculosis. Other diagnostic methods - serological, immunological - are of less importance. Sometimes the diagnosis of tuberculous lesions of the internal genital organs is made during a transsection for suspected space-occupying formations in the area of the uterine appendages.
Treatment genital tuberculosis, as well as tuberculosis of any localization, should be carried out in specialized institutions - anti-tuberculosis hospitals, dispensaries, sanatoriums. Therapy should be comprehensive and include anti-tuberculosis chemotherapy, means of increasing the body's defenses (rest, good nutrition, vitamins), physiotherapy, and surgical treatment as indicated.
The basis of treatment for tuberculosis is chemotherapy using at least three drugs. Chemotherapy is selected individually, taking into account the form of the disease, drug tolerability, and the possible development of drug resistance of Mycobacterium tuberculosis.
It is advisable to include antioxidants (Vitamin E, sodium thiosulfate), immunomodulators (interleukin-2, Methylura-cil *, levamisole), a specific drug tuberculin *, B vitamins, ascorbic acid in the treatment complex.
Surgical treatment is used only for strict indications (tubo-ovarian inflammatory formations, ineffectiveness of conservative therapy for active tuberculosis, formation of fistulas, dysfunction of the pelvic organs associated with pronounced cicatricial changes). Surgery by itself does not lead to a cure, since the tuberculosis infection persists. Chemotherapy should be continued after surgery.
Prevention. Specific prevention of tuberculosis begins in the first days of life with the administration of the BCG vaccine*. Revaccination is carried out at 7, 12, 17 years of age under the control of the Mantoux reaction. Another measure of specificity
Clinical prevention is the isolation of patients with active tuberculosis. Nonspecific prevention involves carrying out general health measures, increasing the body's resistance, and improving living and working conditions.
Acquired immunodeficiency syndrome(AIDS) - a disease caused by the human immunodeficiency virus (HIV). Every year, 3-4 million new cases of infection are registered. In the 25 years since the discovery of the virus, the disease has spread throughout the world. According to statistics, in 2006 more than 25 million people died and 40 million people were registered as HIV-infected (37 million were adults, more than 1/3 of them were women). In Russia, the first case of the disease was noted in 1986. At the moment, about 400 thousand infected people live in Russia, but in reality, according to experts, there are from 800 thousand to 1.5 million people, which is 1-2% of the adult population countries. All the measures that are being taken in the world to stop HIV infection are not bringing results, although they may be curbing its spread.
Etiology and pathogenesis. HIV was discovered in 1983; it belongs to the RNA retrovirus family, a subfamily of lentiviruses (slow viruses). Lentiviral infections are characterized by a long incubation period, low-symptomatic persistence against the background of a pronounced immune response, and cause multi-organ damage with inevitable death. HIV has a unique type of reproduction: thanks to the enzyme revertase, genetic information is transferred from RNA to DNA (reverse transcription mechanism). The synthesized DNA is integrated into the chromosomal apparatus of the affected cell. The target cells for HIV are immunocompetent cells, and primarily helper T lymphocytes (CD-4), since they have receptors on their surface that selectively bind to the virion. The virus also infects some B lymphocytes, monocytes, dendritic cells, and neurons. As a result of damage to the immune system, characterized by a sharp decrease in the number of T-helper cells, an immunodeficiency state occurs with all the ensuing consequences.
The only source of HIV infection is humans. The virus can be isolated from blood, saliva, semen, breast milk, cervical and vaginal mucus, tear fluid and tissues. The most common way the virus spreads (95%) is through unprotected vaginal and anal intercourse. Sufficient permeability of endometrial tissue, vagina, cervix, rectum and urethra to HIV facilitates infection. The danger of anal sexual intercourse is especially great due to the vulnerability of the single-layer epithelium of the rectum and the possible direct entry of the virus into the blood. Homosexuals are one of the main risk groups for AIDS (70-75% of those infected). Sexually transmitted diseases increase the likelihood of HIV transmission due to damage to the epithelial layers of the genitourinary tract.
The vertical route of transmission of HIV infection from mother to fetus occurs both as a result of transplacental transmission (during pregnancy) and through the intranatal mechanism (during childbirth), and postnatally - during breastfeeding.
Parenteral transmission of the virus is possible through contaminated blood or its components, during organ and tissue transplantation, and through the use of unsterile syringes and needles (often among drug addicts).
It has been proven that it is impossible to become infected with HIV through ordinary household contacts, insect bites, food or water.
Clinical picture. Among those infected, young people (30-39 years old) usually predominate. Clinical manifestations are determined by the stage of the disease and concomitant infections.
In the initial stages, half of those infected do not have any symptoms. In 50% of patients, approximately 5-6 weeks after infection, an acute phase develops with fever, general weakness, night sweats, lethargy, loss of appetite, nausea, myalgia, arthralgia, headache, sore throat, diarrhea, swollen lymph nodes, diffuse maculopapular rash, peeling of the skin, exacerbation of seborrheic dermatitis, recurrent herpes.
In the laboratory, primary infection can be confirmed by ELISA methods or by determining specific antibodies (IgG, IgM), as well as DNA and RNA in PCR. Antibodies in the blood usually appear 1-2 months after infection, although in some cases they are not detected even for 6 months or more. Regardless of the presence or absence of symptoms, patients during this period can become a source of infection.
The stage of asymptomatic carriage of HIV can last from several months to several years and occurs regardless of the presence of a febrile stage in the past. There are no symptoms, but the patient is contagious. Antibodies to HIV are detected in the blood.
In the stage of persistent generalized lymphadenopathy, the lymph nodes, primarily the cervical and axillary ones, become enlarged. Candidal lesions of the mucous membranes of the oral cavity and chronic persistent vaginal candidiasis lasting up to 1 year or more are possible.
The stage of development of AIDS (stage of secondary diseases) expresses a crisis of the immune system, an extreme degree of immunodeficiency, which makes the body defenseless against infections and tumors, which are usually safe for immunocompetent individuals. Serious opportunistic infections, the range and aggressiveness of which are increasing, come to the fore. The susceptibility to malignant tumors increases. AIDS-associated infections include Pneumocystis pneumonia, cryptococcosis, recurrent generalized salmonellosis, extrapulmonary tuberculosis, herpetic infection, etc. Secondary infections, together with tumors, determine a wide range of clinical manifestations of AIDS involving all tissue systems in the pathological process. At the last stage of the disease, prolonged (more than 1 month) fever, significant weight loss, damage to the respiratory system (pneumocystis
pneumonia, tuberculosis, cytomegalovirus infection), damage to the gastrointestinal tract (candidal stomatitis, chronic diarrhea). Patients have neurological disorders (progressive dementia, encephalopathy, ataxia, peripheral neuropathy, toxoplasma encephalitis, cerebral lymphoma), skin manifestations (Kaposi's sarcoma, multifocal herpes zoster).
Life expectancy after the first signs of AIDS appear does not exceed 5 years.
The diagnosis of HIV infection is made on the basis of prolonged fever, loss of body weight, enlarged lymph nodes, and AIDS-associated diseases.
Laboratory diagnostics consists of identifying virus-specific antibodies using the ELISA method. If the result is positive, an immunochemical analysis is performed. Additionally, PCR can be used. Antibodies to HIV are necessarily determined in patients during hospital treatment, in pregnant women, donors, in patients at risk, in workers of a number of professions (medics, trade workers, child care institutions, etc.), therefore the diagnosis of HIV infection is established in the early stages in the absence of any - or clinical manifestations. Immunological studies make it possible to assess the degree of immunosuppression and monitor the effectiveness of treatment. For this purpose, the number of T-helpers is determined, as well as the ratio of T-helpers/T-suppressors (CD4/CD8), which steadily decreases as the disease progresses.
Treatment It is recommended to start as early as possible (before deep damage to the immune system) and continue as long as possible. Currently, antiretroviral drugs that suppress viral replication are used: reverse transcriptase inhibitors (zidovudine, phosphazide, zalcitabine, nevirapine) and HIV protease inhibitors (saquinavir, indinavir, ritonavir). Inducers of endogenous interferon are also used. When AIDS-associated diseases develop, appropriate treatment is resorted to. Unfortunately, at present, a complete cure for patients with HIV infection is impossible, but timely treatment can prolong their lives.
Prevention. Since HIV infection cannot be cured radically, prevention becomes the main method of control. Identification of those infected with HIV is of particular importance. Mandatory examination of blood donors, pregnant women, patients with sexually transmitted diseases, homosexuals, drug addicts, and patients with a clinical picture of immunodeficiency is provided. The use of a condom during sexual intercourse with casual or infected partners is strongly recommended. To prevent transmission of infection to the fetus and newborn from a sick mother, the following measures are recommended: use of antiretroviral drugs during pregnancy, delivery by cesarean section and refusal of breastfeeding. If there is a high probability of HIV infection, chemoprophylaxis is indicated. A vaccine against HIV infection is being tested, which will protect a person from becoming infected with the virus.
Control questions
1. The main causative agents of inflammatory diseases of the female genital organs.
2. Classification of inflammatory diseases of the female genital organs according to clinical course and localization of the process.
3. List the factors that contribute to the spread of infection in the genital tract and the ways of its spread.
4. Indicate the factors that prevent infection from entering the genital tract and spreading in the body.
5. Reveal the etiology, pathogenesis, clinical symptoms, diagnosis and principles of treatment of bacterial vaginosis, vaginal candidiasis, trichomonas vaginitis.
6. Describe the etiology, pathogenesis, clinical symptoms, diagnosis and principles of treatment of inflammatory diseases of the internal genital organs.
7. What are the etiology, pathogenesis, clinical picture, diagnosis and principles of treatment of gonorrhea?
Gynecology: textbook / B. I. Baisova et al.; ed. G. M. Savelyeva, V. G. Breusenko. - 4th ed., revised. and additional - 2011. - 432 p. : ill.
